11 Radiation and Radiation Safety
The pre/post questions are listed below. They are all multiple choice questions with a single right answer. To best guide your learning, we have hidden the answers in a collapsible menu. Before reading the chapter, we suggest giving the questions a try, noting your answers on a notepad. After reading the chapter, return to the questions, re-evaluate your answers, and then open the collapsible menu to read the correct answer and discussion. Do not fret if you have difficulty answering the questions before reading the chapter! By the end of the chapter, we are certain you will have covered the knowledge necessary to answer the questions. There will be a teaching case at the end of the chapter. This is another opportunity to exercise your new knowledge!
Pre/Post Questions
Case Based Questions
- A 45 year old vascular surgeon with 10 years of professional practice is preparing to perform a left upper extremity fistulogram due to concerns for prolonged bleeding after hemodialysis. What is the most appropriate PPE that the student should wear during the case?
Full leaded face shield, lead apron, and personal radiation badge
Lead apron alone
Leaded safety glasses
Lower half of a 2-piece lead apron and thyroid shield
Lead apron, leaded safety glasses
- A 25 year old medical student has been invited to observe endovascular stent placement for an infrarenal AAA. In addition to wearing appropriate PPE, what can the medical student do to reduce their exposure during the case?
Stand as close to the radiation source as possible.
Turn their back to the radiation source.
Stand as far from the radiation source as possible.
Wear a radiation badge.
- A 55 year old vascular surgeon who has been practicing for 20 years has noticed some subtle changes in his vision. What is the most likely underlying disease process?
Optical neuropathy
Glaucoma
Opacification of the lens
Retinal angiopathy
- A 65 year old female is presenting to the hospital for endovascular repair of a complicated AAA. There is prolonged radiation time with a calculated absorbed dose of 3.5 Gy. What is the most likely skin exam finding during the patient’s hospital course?
Skin necrosis
Burn
No acute findings as the dose were too low
Erythema
- A 42 year old male on hemodialysis from a left upper extremity brachiocephalic fistula for CKD is seen for a fistulogram due the patient having trouble pulling during dialysis. The patient is placed in the supine position with left arm extended. The c-arm is initially perpendicular to the operating table. To achieve better views of the proximal vessels, the c-arm is rotated counterclockwise (from the perspective of looking from the patient’s feet superiorly) so that the image intensifier is rotated more towards the patient’s right shoulder. What is the appropriate name for the c-arm position?
LAO (left anterior oblique)
RAO (right anterior oblique)
Cranial
Caudal
AP (anterior posterior)
- A 27 year old female who is a circulating nurse in the endovascular suite recently became pregnant. She has informed the radiation safety officer and staff of the endovascular suite. She is curious how best to monitor the radiation dose the fetus is receiving in utero. Where should the nurse place the fetal dosimetry badge?
The dosimetry badge should be worn on the outside of the lead apron at chest level
The dosimetry badge should be worn under the lead apron around chest
The dosimetry badge should be worn outside the lead apron at the abdomen level.
The dosimetry badge should be worn under the lead apron at the abdomen level.
Introduction
The use of radiation is fundamental to a vascular surgeon’s practice. Intraoperative fluoroscopy, computer tomography (CT), and plain film X-rays (to a lesser extent) are crucial tools in vascular surgery. The vascular surgery patient will likely undergo all these radiation-based imaging studies.
Vascular surgeons and other professionals (nurses, scrub technicians, imaging technicians, etc.) can be exposed to significant levels of radiation over a career of performing intraoperative fluoroscopy/angiography and endovascular surgery. As the medical community is well aware of these risks, many initiatives are underway to decrease the amount of radiation required to perform studies and interventions.
Vascular patients are also exposed to radiation, although often at higher doses over shorter periods of time. Educating oneself about radiation and radiation safety is essential. This chapter will explore the basics of radiation, radiation safety principles and measures, and potential adverse outcomes of significant radiation exposure.
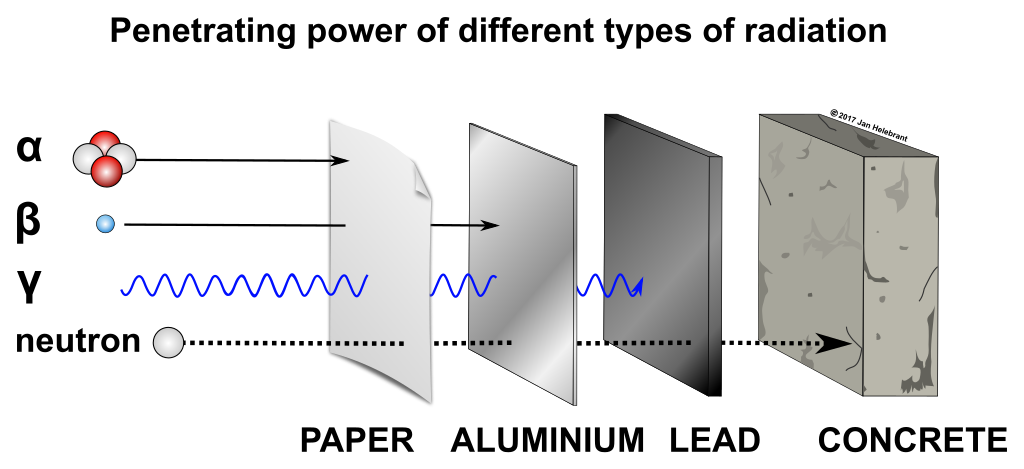
Radiation Penetrance
A critical concept to understand when discussing occupational and patient exposure to radiation is penetrance.
- Penetrance refers to the ability of emitted radiation to penetrate into or through materials and is defined as the fraction of radiation passing through a given object (or the inverse of attenuation).
- The density of materials or tissues determines their ability to attenuate or block X-rays.
- Dense tissues (bone) or materials (lead) absorb a greater fraction of radiation while less dense tissues (skin) or materials (water) allow for deeper penetration.
This concept is especially relevant to vascular surgeons and their patients as an increasing proportion of vascular procedures are performed endovascularly under live fluoroscopy which utilizes X-rays.
Radiation types
Radiation can be broadly categorized into ionizing and non-ionizing forms. This chapter will focus on ionizing radiation, which is encountered by medical professionals in clinical settings.
Ionizing radiation falls within the higher frequency range of the electromagnetic spectrum. The commonly discussed types of ionizing radiation include X-rays, alpha particles, beta particles, gamma rays.
Alpha Particles
Alpha particles, despite their high energy, have poor penetrance. As such, they do not penetrate the skin. However, they can be dangerous if inhaled or ingested.
Beta Particles
Beta particles, have slightly more penetration than alpha particles.
They have some ability to penetrate the skin. However, they can be easily blocked by less dense shielding like aluminum.
Similar to alpha particles, beta particles can also cause harm if ingested or inhaled.
Gamma Rays
Gamma rays possess significantly more energy and can penetrate through the human body and less dense shielding.
Lead is effective in shielding against gamma rays due to its density. Dense materials increase the likelihood of radiation interacting with subatomic particles, reducing the rays’ passage through the material.
As gamma rays pass through the body, they cause ionizing damage to tissue and DNA and should be treated with caution.
X-Rays
X-rays, widely used in healthcare, share similarities with gamma rays in their ability to penetrate tissue.
Their application in medical imaging includes plain X-ray films, CT scans, and fluoroscopy.
Lead is effective in shielding against x-rays due to its density.
The position of the x-ray emitting source of the the C-arm used for endovascular procedures is at the bottom of the arm, beneath the patient and the operating room table. This is the location of highest exposure.
As the X-ray source emits radiation, radiation scatter occurs, moving upward and outward from the source.
Terminology
It is imporant to understanding the terminology related to radiation exposure.
- The absorbed dose refers to the energy from ionizing radiation per unit mass of exposed material, measured in grays (Gy).
- The equivalent dose represents the mean absorbed dose of a specific organ or tissue, measured in sieverts (Sv).
- The effective dose, also measured in *8sieverts (Sv),** accounts for total-body radiation exposure and is guided by the International Commission on Radiological Protection (ICRP) guidelines for comparing radiation effects on individuals.
X-ray technology for imaging comprises two critical components: the radiation source, where X-ray photons are generated, and the detector.
- The shape of the beam from the source is managed by the collimator.
- As X-ray beam passes through the patient, they are captured by the detector and an image is created by image intensifier.
In endovascular procedures using a C-arm, the detector portion (i.e. image intensifier) is above the patient, while the X-ray source is beneath the patient and table.
Principles for Patient Safety and Radiation Exposure
While any procedure that produces ionizing radiation will expose the patient to some degree of risk, it is the responsibility of the patient’s surgeon to ensure that the risk of the procedure is minimized as much as possible without compromising the efficacy of the therapy.
Certain considerations exist for special patient populations including pregnant patients. These are discussed later in this chapter.
A number of core principles should be considered whenever a provider is considering recommending or performing a treatment with ionizing radiation including:
Medical Necessity and Justification for the Procedure
The potential benefits of the procedure should outweigh the risks of not performing the procedure or performing an alternative procedure without radiation exposure.
Exposure Optimization
The radiation dose delivered, particularly for intraoperative exposures, should be optimized to be as low as possible while still achieving adequate image quality for the procedure and decision making.
This includes fluoroscopy techniques such as reducing the time under fluoroscopy by using pulsed fluoroscopy as opposed to continuous scanning, collimating the X-ray beam to the area of interest and narrowing the beam to only scan structures necessary, adjusting the frame rate of fluoroscopy images when temporal resolution is not necessary.
It also includes effective preoperative planning, including properly positioning the patient for optimal imaging to reduce repeated attempts, and planning with previous imaging to ensure good understanding of the vascular anatomy and to form a procedural plan prior to exposing the patient to additional radiation.
The ALARA Principles
ALARA stands for “As Low As Reasonably Possible,” and refers to the balance between minimizing radiation exposure to the patient without compromising the quality of care.
The energy of the X-rays: Higher energy X-rays will have greater penetrance and pass through thicker and deeper tissue more easily. Energy is typically adjusted during the procedure to optimize for the depth of the structures being imaged.
The duration of exposure: The dose of radiation delivered to the patient and the OR staff is directly correlated with the duration of exposure. This is why vascular surgeons try to limit the amount of time under fluoroscopy to the minimum required.
The distance from the source: The intensity of radiation exposure decreases with distance from the emitting source in an inverse square relationship. The patient and surgeons at bedside and closest to the C-arm, therefore, receive significantly greater doses of radiation as compared to OR staff further away.
Patient Education and Informed Consent:
Patients should be informed about the risks of exposure to ionizing radiation, the benefits of the procedure, and the efforts made to reduce total dosage.
Patients should provide informed consent before any intervention whenever possible, and should be encouraged to ask questions and voice concerns prior to the initiation of treatment.
Patient monitoring and dose recording:
During fluoroscopy-guided procedures, patient radiation doses should be monitored and recorded accurately to help understand the patient’s cumulative radiation exposure.
In a hybrid OR, the total radiation is recorded on the large screen. If not, you can always ask the hybrid room technician.
Radiation shielding:
The use of personal protective devices made of dense materials, such as lead aprons, thyroid collars, and other protective shields, serve to attenuate radiation.
Shielding
Shielding serves to protect vital organs from radiation exposure and damage. The most common type of shielding is lead, typically in the form of a skirt, vest, and thyroid shield worn beneath the surgical gown.
Lead aprons and other lead-lined materials are highly effective in protecting personnel from radiation exposure. Lead, being a very dense material, absorbs a significant portion of the radiation from X-ray beams that would otherwise reach the person wearing it. These lead protection devices are specifically designed to safeguard vital organs and those most sensitive to radiation exposure—such as organs not shielded by overlying bone. This includes the torso, reproductive organs, and the thyroid gland.
Reported effectiveness of worn lead varies. Some sources claim that a lead apron with a thickness of 0.5 mm can reduce radiation scatter by 90%, while others suggest a lesser reduction. However, there is a consensus that the apron should be at least 0.25 mm thick both in the front and back. (Cheon et al. 2018)
Additional shielding such as lead screens can be found in the OR to provide further protection against scattered X-rays.
Please find an examples of lead shields here:
Radiation Badges
Radiation badges or “dosimeters” are personal wearable devices designed to measure the amount of radiation exposure an individual receives. They measure the total exposure accumulated over a set period of time. It’s important to note that these devices specifically measure ionizing radiation and not other forms.
There are several types of badges available. Film badges are commonly used in clinical practice. They are worn by a single person and are evaluated every 30 days. Other types of badges provide real-time quantification of radiation exposure, with readings recorded at the beginning and end of each shift. A radiation officer is typically tasked with tracking these exposure levels.
Please find more information about radiation badges here:
When an individual’s exposure approaches a certain threshold, which is typically set below the maximum allowable dose for a year, measures are taken to further minimize their exposure. For instance, if an employee has reached a significant exposure level two months into the year, the radiation compliance officer would discuss strategies to reduce their exposure. Strategies include maintaining greater distance from radiation sources, rotating through cases more frequently, and avoiding involvement in procedures with a higher risk of elevated radiation levels.
If an employee surpasses their annual exposure limits, they are typically prohibited from participating in procedures involving radiation for the remainder of the year. The specific limits of exposure are detailed later in the chapter.
Lead Glasses and Eye Protection
In the endovascular suite, it’s common to see individuals wearing leaded glasses. A 2016 study compared different types of glasses and their effectiveness in reducing radiation exposure. The results showed that all leaded glasses outperformed non-leaded safety glasses, with an average reduction in dose of approximately 90.3%. (Waddell et al. 2016) This study is just one of many that highlight the efficacy of lead glasses in minimizing eye exposure during procedures involving radiation.
Despite the significant reduction achieved with the use of lead safety glasses, there’s a caveat regarding a false sense of security. Due to the scattering of radiation during procedures, the eye can be exposed to radiation at oblique angles (i.e. around the glasses), leading to increased exposure and limited reduction in dose. (Kirkwood et al. 2020) In such scenarios, the optimal solution for reducing eye exposure would be a full visor or face shield with lateral eye shielding. A study by Samara et al. demonstrated that the most substantial dose reduction was observed in the full visor group.(Samara et al. 2022)
Wearing lead safety glasses during interventions is recommended as it reduces radiation exposure and helps maintain eye health, particularly for individuals at risk of accumulating significant lifetime radiation exposure.
Please find an examples of lead glasses here:
Imaging Technique
Now that we’ve covered both radiation equipment and safety gear, it’s crucial to underscore the importance of imaging technique. This concept is critical because it addresses the multifaceted aspects of minimizing radiation exposure during procedures.
The radiation dose depends on both the intensity of imaging and the duration of fluoroscopic exposure. (Rial and Vañó 2021) During endovascular procedures, the operating surgeon can control these factors by:
Pulse imaging: Instead of continuously scanning the patient, the surgeon can pulsate images (i.e. shoot several plain x-rays). This approach reduces scatter and lowers overall exposure. It’s especially effective when high temporal resolution isn’t necessary.
Collimator use: The surgeon can use the collimator to narrow the X-ray beam, focusing solely on the area of interest. This method effectively reduces both dose and scatter.
The image intensifier should be positioned closer to the patient to optimize image quality. Conversely, the X-ray tube should be placed further away from the area being imaged.
If the X-ray tube is too close, imaging quality can degrade and radiation dose increases. This strategic arrangement ensures that the image quality remains high while minimizing patient exposure to radiation.
See a visual summary of correct and incorrect technique here.
Another crucial aspect of radiation exposure is a person’s distance from the radiation source. Radiation exposure decreases as the distance from the source increases. This phenomenon follows an inverse square law (1/d^2). (Kim 2018)
Suppose a medical student is initially one foot away from a radiation source, and their exposure is measured at 500 mGy/min. If they then move ten feet away from the source, their exposure would reduce significantly to 5 mGy/min. This example vividly demonstrates why distance from the source plays a pivotal role in minimizing radiation exposure.
See a visual summary of the inverse square law and distance from radiation source here.
If you are not scrubbed, the ideal place to stand is as far away from the x-ray source while making sure you can still see the images and interact with the surgical team.
When discussing the positioning of the C-arm, it’s useful to become familiar with some common terminology. To improve visualization of the target area, the C-arm can rotate left and right, and cranially or caudally. All terminology is relative to the radiation source (under the table) and not the intensifier (above the patient). Two frequently encountered positions are RAO (right anterior oblique) and LAO (left anterior oblique).
See a visual summary of C-arm rotation here.
Adverse Outcomes Given Prolonged Radiation Exposure
Limits
Various governing agencies in the US and around the world have established limits on yearly radiation exposure.
Currently, the United States Occupational Safety and Health Administration, Nuclear Regulatory Commissions, and Department of Energy all stipulate a yearly limit of 5,000 mrem/year (50 Sv). [“Radiation In Perspective” (n.d.)](“Information for Radiation Workers,” n.d.)
Some agencies further specify this limit to 1,250 mrem/quarter (12.5 Sv). (“Radiation Emergency Preparedness and Response - Response | Occupational Safety and Health Administration,” n.d.)
Deterministic versus stochastic radiation effects
Before delving into the various risks associated with radiation exposure, it’s essential to provide a brief overview of the types of radiation effects. These effects can be broadly categorized into deterministic and stochastic effects.
Deterministic effects, also known as non-stochastic effects, occur when specific radiation dose thresholds are exceeded leading to adverse outcomes. They are dose-dependent and result in significant damage, such as cell death in a specific organ. Examples of deterministic effects include cataracts, infertility, and non-malignant skin lesions. (Weerakkody et al. 2008a) Making sure thresholds are not surpassed is pertinent not only for individuals working in the endovascular suite but also for ensuring patient safety.
The table below outlines the various adverse deterministic (non-stochastic) effects associated with radiation doses in comparison to the average exposure during endovascular aneurysm repair (EVAR).(Weerakkody et al. 2008a)
Radiation absorbed dose and associated side effect compared to EVAR
| System | Side Effect | Source | Dose (Gy) | Average EVAR dose (Gy) [31] |
|---|---|---|---|---|
| Integumentary | Early transient erythema | Stewart, et. al. | Single dose: 2 | .85 median (interquartile range .51 - 3.74) |
| Burns | Williams | Single dose: 5-10 | ” | |
| Reproductive | Sterility | Williams | Single dose: 3-6 | ” |
| Thyroid | Hypothyroidism | Nagayama | Cumulative dose High dose: 15-44 Low dose: variable | ” |
| Ocular | Cataracts | Williams, et. al. | Single dose .5 | ” |
The table above underscores a crucial consideration: deterministic effects may potentially arise in cases with prolonged run times. Endovascular aneurysm repair (EVAR) is a routine procedure for modern vascular surgeons. While the duration of these procedures may vary, considering the cited range of radiation dosages from 0.51 to 3.74 (Weerakkody et al. 2008a), it’s conceivable that patients could experience post-operative adverse events solely due to the effects of radiation exposure.
In contrast, stochastic effects result from repeated exposure to radiation levels below a certain threshold. A notable example of stochastic effects is cancer. Stochastic effects are probabilistic in nature. For example, the likelihood of developing leukemia after a single chest X-ray is low. However, if someone were to undergo a head-to-toe CT scan daily for a year, the probability of developing leukemia would significantly increase, even though there isn’t a direct correlation between the dose of radiation and the observed effect. (Hamada and Fujimichi 2014)
The Eye and Radiation Exposure:
During radiological procedures, one organ that often goes unnoticed but is significantly exposed is the eye, specifically the lens.
The lens of the eye is particularly sensitive to radiation .
Cataracts: Prolonged exposure to significant radiation levels can lead to opacification of the lens (i.e. cataracts)
This gradual process ultimately results in the development of cataracts, with the most common subtype being posterior subcapsular (PSC) cataracts. (Loganovsky et al. 2020)
A study conducted in 2013 examined the dose-effect relationship of radiation on the eyes of interventional cardiologists and electrophysiologists. The study found that up to 25% of the physicians involved had exceeded current exposure thresholds and were at risk of developing radiation-induced cataracts. (Jacob et al. 2012)
Other ocular pathologies associated with radiation exposure include:
Cataracts: Prolonged exposure to radiation may lead to the development of cataracts, causing clouding of the lens.
Glaucoma: Radiation exposure can contribute to glaucoma, a condition characterized by increased intraocular pressure.
Optic Neuropathy: Damage to the optic nerve due to radiation exposure can result in vision impairment.
Retinal Angiopathy: Radiation may impact retinal blood vessels, leading to angiopathy.
Dry Eye Syndrome: Radiation exposure can cause dryness and discomfort in the eyes.
In recent years, there has been growing research interest in understanding the potential adverse effects of long-term radiation exposure on ocular health.
The increased understanding of these risks has prompted a greater emphasis on the importance of safety equipment to protect the eyes. Proper use of protective gear such as lead glasses and face shields is crucial for minimizing radiation exposure to ocular tissues.
The Skin and Radiation Exposure:
Skin changes of varying severity are a well-documented adverse reaction to radiation exposure. These changes can range from mild redness and irritation to severe necrosis and the development of secondary skin cancers. Importantly, these changes may not always manifest immediately.
Adverse effects to the skin vary according to the cumulative dose of radiation. For example, at the large cumulative dose of 50 Gy, fibrosis may occur, presenting as induration, skin retraction, edema, restricted motion, ulceration, and necrosis. (Bennardo et al. 2021) This underscores the importance of understanding a patient’s radiation exposure history, as it could increase their susceptibility to radiation-induced injury.
The most commonly encountered adverse skin effect is acute radiation dermatitis.
Acute radiation dermatitis characterized by redness and ulceration, can occur with relatively low doses, such as 2 Gy. [Stewart et al. (2012)](Bennardo et al. 2021)
This level of exposure is concerning not only for individuals undergoing routine radiation therapy for cancer treatment but also for those in prolonged surgeries requiring fluoroscopy, as highlighted in Weerakkody’s study on endovascular aneurysm repair (EVAR). (Weerakkody et al. 2008b)
Symptoms of acute radiation dermatitis typically appear within 2 to 24 hours following exposure.
As the radiation dose increases, the severity of side effects worsens, and the time to onset of these effects also lengthens. For instance, a single radiation dose of 10 Gy may result in dermal atrophy, but this may not be evident until more than 10 weeks after exposure. (Stewart et al. 2012)
This discussion doesn’t cover all possible adverse effects related to skin radiation exposure. Rather, it provides an overview of common findings based on typical exposure scenarios in vascular surgery patients. Further information on the effects of single and cumulative radiation doses on the skin can be found in studies by Stewart ((Stewart et al. 2012)) and Bennardo ((Bennardo et al. 2021)), respectively.
Thyroid Dysfunction, Thyroid Cancer, and Radiation Exposure
It is widely acknowledged that radiation exposure during childhood significantly increases the risk of developing thyroid cancer. Key risk factors in this context include both the dose of radiation received and the age at the time of exposure.(Iglesias et al. 2017) However, when it comes to establishing a similar relationship in adulthood, the evidence has been less straightforward.
In October 2023, The Journal of Radiation Research published a systematic review and meta-analysis specifically examining the incidence of thyroid cancer following radiation exposure in adults. While some studies suggested an increased risk of cancer in adults exposed to radiation, the relative risk at a dose of 10 mGy (milligray) was deemed insignificant. In other words, the risk did not show a significant elevation at this particular dose level.
While a definitive link between radiation exposure and thyroid cancer in adult populations remains elusive, several studies have hinted at a potential association between low-dose ionizing radiation and thyroid dysfunction.
- There have been reports of hypothyroidism marked by elevated levels of thyroid-stimulating hormone (TSH) and lower-than-average levels of free triiodothyronine (T3) and thyroxine (T4) compared to unexposed individuals. (Cioffi et al. 2020)
Given the potential implications of radiation exposure to thyroid disfunction and cancer, additional research into the long-term effects of ionizing radiation exposure on thyroid function is warranted. Numerous studies have emphasized the need for further investigation in this area.
Reproductive Function and Radiation Exposure
One of the significant concerns associated with radiation exposure is its impact on reproductive health.
In the female reproductive system, ionizing radiation primarily affects the ovaries, potentially leading to:
1. Ovarian Insufficiency: Prolonged exposure to radiation may result in ovarian insufficiency, affecting the ovaries’ ability to function optimally.
2. Delayed Puberty: Radiation exposure can also contribute to delayed puberty in females.
3. Infertility: Ultimately, these effects may culminate in infertility.
Some sources suggest that radiation to the head during routine medical procedures could disrupt the hypothalamic-pituitary-gonadal (HPG) axis. (Marci et al. 2018) This disruption may lead to hormonal dysregulation, further impacting reproductive health.
Radiation exposure to male reproductive organs can disrupt spermatogenesis, depending on the stage of sperm development. The damage from ionizing radiation may lead to decreased sperm motility, increased fragmentation, and DNA alterations. (Wdowiak et al. 2019)
Hematologic Disease and Radiation Exposure
Prolonged low-dose radiation exposure has the potential to cause serious hematological effects. Numerous studies, including those conducted outside the medical field, have examined hematologicaly consequences of employees at risk of radiation exposure.
A particularly noteworthy study, published in 2015, involved an international cohort of observers within the nuclear industry. Their research revealed compelling evidence linking low-dose radiation exposure to the development of non-chronic lymphocytic leukemia (CLL). (Leuraud et al. 2015)
Specifically, the study highlighted a direct correlation between cumulative red bone marrow dose over a two-year period and the excess relative risk of developing leukemia.
Their findings indicated that the relative risk of leukemia mortality was approximately 2.96 per Gy of exposure (RR = 2.94 per Gy).
While we won’t delve into the intricate details of these findings in this chapter, they underscore the critical importance of considering lifelong radiation exposure and the need for effective protective measures.
Pregnant Populations
When it comes to radiation exposure during pregnancy, there are important guidelines and considerations to keep in mind.
To monitor the radiation dose absorbed by the fetus, a dosimeter or radiation badge is typically worn under the lead apron at the level of the abdomen.
This dosimeter is checked monthly, and the absorbed dose is calculated accordingly.
Fetal Harm Threshold: Ensure that the radiation dose does not exceed 0.5 mSv per month or a maximum fetal dose of 5 mSv throughout the entire pregnancy
The following table adapted from a study by Vu et al. ((Elder and Vu 2013)) summarizes the deterministic effects of radiation during pregnancy.
| Deterministic effect | Gestation (weeks) | Threshold dose (mGy) |
|---|---|---|
| Embryonic death | 3 – 4 | 100 – 200 |
| Major malformations | 4 – 8 | 250 – 500 |
| Growth retardation | 4 – 8 | 200 – 500 |
| Irreversible whole body growth retardation | 8 – 15 | 250 – 500 |
| Severe mental disability | 8 – 15 >16 | 60 – 500 >1,500 |
| Microcephaly | 8 – 15 | >20,000 |
| Decrease in intelligence quotient | >16 | >100 |
Lead Thickness Considerations for Pregnant Providers:
Minimum Thickness: Pregnant individuals should wear a lead apron with a minimum thickness of 0.5 mm. This ensures proper coverage of the abdomen, shielding the fetus from radiation exposure.
Double-Thickness Option: Alternatively, a double-thickness lead apron (1.0 mm) can be worn. According to Vu et al. ((Elder and Vu 2013)), this reduces the absorbed dose from 9 mrem to 3 mrem.
Weight Consideration: However, it’s essential to recognize that wearing a thicker lead apron may increase the risk of back injury due to the added weight. Balancing protection and comfort is crucial.
As always, healthcare providers should adhere to the ALARA principles outlined above (i.e. maintaining a maximum reasonable distance from the source, using the collimator, pulse imaging, etc.).
Teaching Case
Scenario
A 75-year-old male is scheduled for an angiogram of the left lower extremity to investigate and potentially treat claudication symptoms. The attending vascular surgeon, with over 25 years of experience in endovascular therapy, takes precautionary measures by wearing a thyroid shield, prescription glasses, and a 2-piece lead apron. However, due to challenges in navigating the stenosed arterial system, the fluoroscopy time during the procedure was extended. Subsequently, the calculated radiation dose amounted to 3 Gy.
Discussion Points
However, we feel this chapter contains all the necessary information to answer the questions. If not, please let us know!
- What could be done to reduce the dose of radiation to the surgeon?
- What could be done to reduce the dose of radiation to the OR staff?
- What gaps are present in the surgeon’s PPE?
- What are some potential adverse effects of prolonged radiation exposure to the surgeon?
- Given the level of radiation, what adverse effects might be noted in the patient?
- If the case were to progress longer, what might be the subsequent adverse outcomes to the patient?
Key Articles
- Mitchell EL, Furey P. Prevention of radiation injury from medical imaging. J Vasc Surg. 2011 Jan;53(1 Suppl):22S-27S. doi: 10.1016/j.jvs.2010.05.139. Epub 2010 Sep 16. PMID: 20843625. (Mitchell and Furey 2011)
Additional Resources
Audible Bleeding Content
- Audible Bleeding Exam Prep: Radiation Safety
- Special Topic: Occupational Hazards for the Vascular Surgeon. Listen to the episode below and find additional information here, or find the episode wherever you listen to podcasts.
- JVS Author Spotlight - Jasmine Bhinder, MD. Listen to the episode below and find additional information here, or find the episode wherever you listen to podcasts.
Gore Combat Manual
The Gore Medical Vascular and Endovascular Surgery Combat Manual is an informative and entertaining read intended as a vascular surgery crash course for medical students, residents, and fellows alike. Highly accessible with a thoughtfully determined level of detail, but lacking in learning activities (e.g. questions, videos, etc.), this resource is a wonderful complement to the APDVS eBook.
Please see pages 43-46.